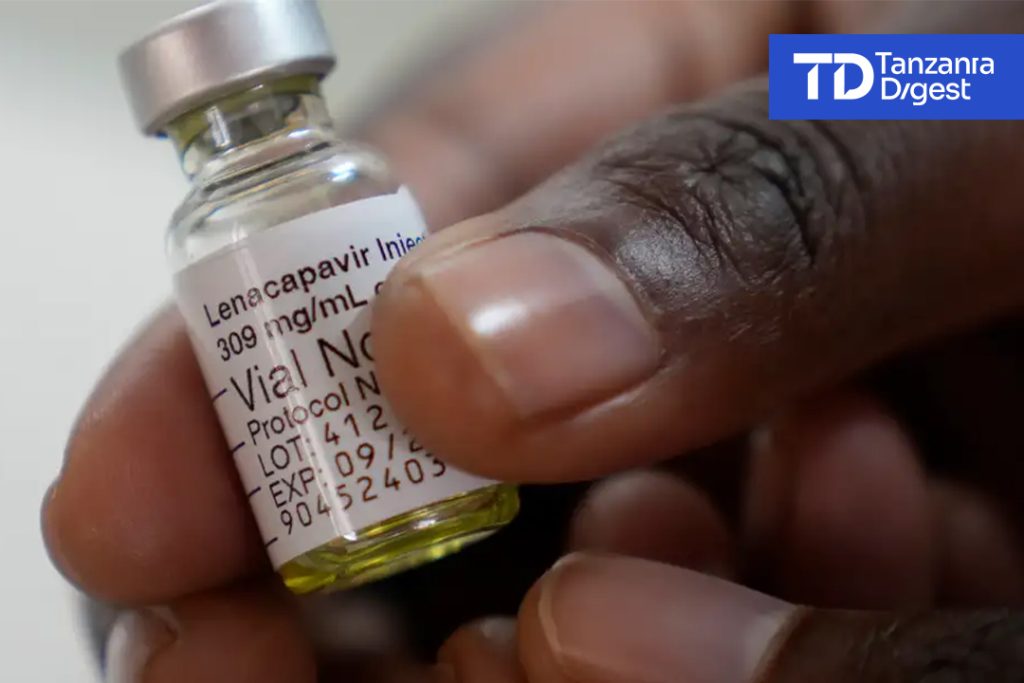
Lenacapavir is the latest HIV preventive injection administered twice a year. From successful clinical tests, we learnt that Initially, lenacapavir, was aimed to resolve drug resistances of HIV and AIDS patients.
However, it developed to be 100% effective in preventing HIV in one trial and 96% in the other. Drugs are still widely used to prevent HIV transmission but have faced amnesia leading to patients failing to keep up with the daily intake schedule.
Moreover, drugs carry stigma and tend to develop drug resistances while other patients complain of stomach upsets and other significant side effects. Lenacapavir which essentially is an HIV inhibitor injection taken biannually is also confounded by short term known side effects and unknown long term side effects.
Apart from inherent medical issues, the injection isn’t a vaccine as many had anticipated. It only interferes in the life cycle in the development of HIV virus making it extremely difficult to blossom in the human body. It is a huge relief once you consider how many people have died because of HIV & AIDS.
We know lenacapavir isn’t that silver bullet to this global pandemic but effectively slows the transmission of HIV. US president Donald Trump campaigned on the platform of lowering prescription costs, and Medical research complained it will reduce incentive to carry out costly research most of which don’t pay up for themselves.
Is lenacapavir a step forward for all of us? What is the future stand to find the panacea of HIV through an effective vaccine? Will AI have a role in finding both the cure and the vaccine?
🚀 Lenacapavir: A Transformative Leap in HIV Prevention with Persistent Challenges.
💉 1. Breakthrough Efficacy and Mechanism.
– Unprecedented Effectiveness:
In Phase 3 trials (PURPOSE 1 and 2), twice-yearly lenacapavir demonstrated “100% efficacy” in preventing HIV among cisgender women in sub-Saharan Africa and “96% efficacy” among cisgender men, transgender individuals, and gender-diverse populations. This surpasses daily oral PrEP (e.g., Truvada), which relies on consistent adherence and shows real-world effectiveness as low as **26%** in some groups due to missed doses.
– Innovative Action:
As a “capsid inhibitor”Lenacapavir disrupts HIV’s capsid protein, blocking multiple stages of the viral life cycle. Unlike vaccines, it does not stimulate immune memory but acts as a biologic “shield” with “no known cross-resistance” to other drug classes. Its biannual dosing overcomes adherence barriers linked to stigma and forgetfulness.
⚠️ 2. Hurdles to Widespread Adoption.
– Short-Term Safety:
Injection-site reactions (e.g., nodules, pain) occurred in “18%” of trial participants, leading some to discontinue treatment. Most were mild, but severe cases were linked to improper injection technique. “Long-term effects” remain unknown, necessitating ongoing surveillance.
– Drug Resistance Risks:
If administered to individuals with undiagnosed HIV, lenacapavir monotherapy could foster “drug-resistant strains”. Rigorous HIV testing before each injection is mandated to mitigate this.
– Cost and Access Inequity:
– The U.S. list price is “l~$28,000/year”, potentially limiting access in resource-limited regions.
– Gilead’s access strategy includes:
– “Generic licensing” for 120 low-income countries (royalty-free).
– “Donation programs” for 2 million people.
– “Excluded middle-income countries” (e.g., Mexico, Brazil) may face affordability gaps without tiered pricing.
– Funding Threats:
Recent U.S. cuts to HIV research programs (e.g., termination of “CHAVD consortia” and “USAID’s BRILLIANT trial”) jeopardize rollout support and future innovations.
🔮 HIV Vaccine Research: Progress Amid Uncertainty.
💉 1. Current Vaccine Breakthroughs.
– Germline Targeting Success:
Recent trials (IAVI G002/G003) used “mRNA-delivered immunogens” to activate B-cells capable of producing broadly neutralizing antibodies (bnAbs). In North American and African participants, “94–100%” developed early-stage bnAb precursors after priming doses. Heterologous boosting further matured these responses, marking a “critical proof-of-concept”.
– Platform Advantages:
mRNA technology enables rapid iteration of immunogens, accelerating vaccine design against HIV’s hyper-variable strains.
🛑 2. Funding Crisis and Setbacks.
– NIH/CHAVD Termination:
The cancellation of “$258 million in grants” for leading consortia (Scripps/Duke) halts upcoming trials of bnAb-based vaccines, delaying potential efficacy studies by years.
– Global Ripple Effects:
Cuts to foreign subawards and mRNA initiatives (e.g., H5N1 vaccine contracts) stifle low-income country trials essential for studying region-specific HIV strains. As one scientist lamented:
> “We’re at a point of more progress than ever… This is a sad development obstructing forward progress” – Dennis Burton, Scripps.
🤖 AI in HIV Research: Accelerating Cures and Vaccines
🔍 1. Current AI Applications.
– Drug Discovery:
AI models screen compounds for “multi-target inhibitors” (e.g., candidates effective against both HIV and hepatitis C). For capsid inhibitors like lenacapavir, AI predicts binding affinities by analyzing van der Waals interactions and residue contacts.
– Diagnostic Enhancements:
Deep learning algorithms interpret “HIV self-test images” with “97.8% sensitivity” (outperforming humans in detecting faint lines), reducing false negatives in rural settings.
– Viral Integration Analysis:
Tools like “DeepHINT” use attention-based networks to predict HIV integration sites in the human genome, revealing mechanisms of viral persistence.
🚀 2. Future Potential.
– Vaccine Design:
AI can map “B-cell receptor sequences” from single-cell data to engineer immunogens that elicit bnAbs. Combined with mRNA platforms, this may overcome HIV’s variability.
– Cure Research:
AI identifies “latency-reversing agents” to flush HIV from reservoirs and designs gene therapies targeting proviral DNA.
– Barriers:
Data scarcity (due to privacy concerns) and poor model interpretability remain challenges.
💎 Conclusion: A Step Forward, Not a Panacea.
Lenacapavir represents a “paradigm shift in HIV prevention”, offering unparalleled efficacy and convenience. However, its impact hinges on addressing “cost barriers, injection logistics, and political will”. Meanwhile, HIV vaccine research advances but faces “existential funding threats”.
AI emerges as a pivotal ally, yet requires sustained investment to unlock cures. As the fight against HIV evolves, these parallel strides—biomedical, political, and technological—must converge to end the pandemic by 2030.
> “Science is the engine of humanity, but policy and equity are its fuel.”– Adapted from IAVI CEO Mark Feinberg.
Read more analysis by Rutashubanyuma Nestory